A mum with ulcerative colitis says finding an effective medication has transformed her life as a major study shows advanced therapies are cutting the need for surgery.
Retired midwife Emma Louise Jamie said the bowel condition had “taken over” her life since she began experiencing issues a decade ago.
“I started to have cramps, urgency, needing to go to the toilet very frequently – and it would come from nowhere,” she said.
“I would be fine, then I’d go out for a meal and immediately need to go to the toilet afterwards. If I ate anything, it would come straight out.
“I knew all the toilets around Princes Street, or if we were going on a journey, I needed to know where toilet stops were.”
Emma, who was eventually diagnosed with ulcerative colitis after years of symptoms, said the diagnosis initially came as a relief.
“I honestly thought I had cancer, so I thought, ‘I can deal with UC,’” she said. “I didn’t know at that point how much it would affect my life.”
 STV News
STV NewsUlcerative colitis is a form of inflammatory bowel disease (IBD) that affects around one in every 100 people in Scotland and around 300,000 across the UK.
The condition causes chronic inflammation of the colon and rectum, leading to symptoms such as abdominal pain, diarrhoea, fatigue, and weight loss.
In severe cases, it can require surgery to remove the large intestine – a life-changing operation known as a colectomy that often sees patients fitted with a stoma.
For years, Emma tried steroids, enemas, and other medications that only offered temporary relief before they stopped taking effect. At her lowest point in 2019, she was going to the toilet 70 times a week.
“I was feeling absolutely exhausted, living life just to work and be with my family. But they were often caring for me rather than me caring for them.
But in recent years, Emma was prescribed an advanced therapy Infliximab – an IV infusion that targets the specific immune system processes responsible for inflammation.
She receives an injection every six weeks, alongside Mercaptopurine tablets and the anti-inflammatory drug Pentasa.
Since then, she has seen what she describes as a “tenfold” improvement in her symptoms.
“It’s amazing,” she said. “We have a caravan and often go away. I went skiing with my son for a week – I skied every day. My brother-in-law said, ‘You wouldn’t have been able to do this a few years ago.’ It’s changed my life completely.”
Her story mirrors findings from a new study by the University of Edinburgh, which shows that better access to advanced therapies is significantly reducing the number of patients needing surgery for ulcerative colitis.
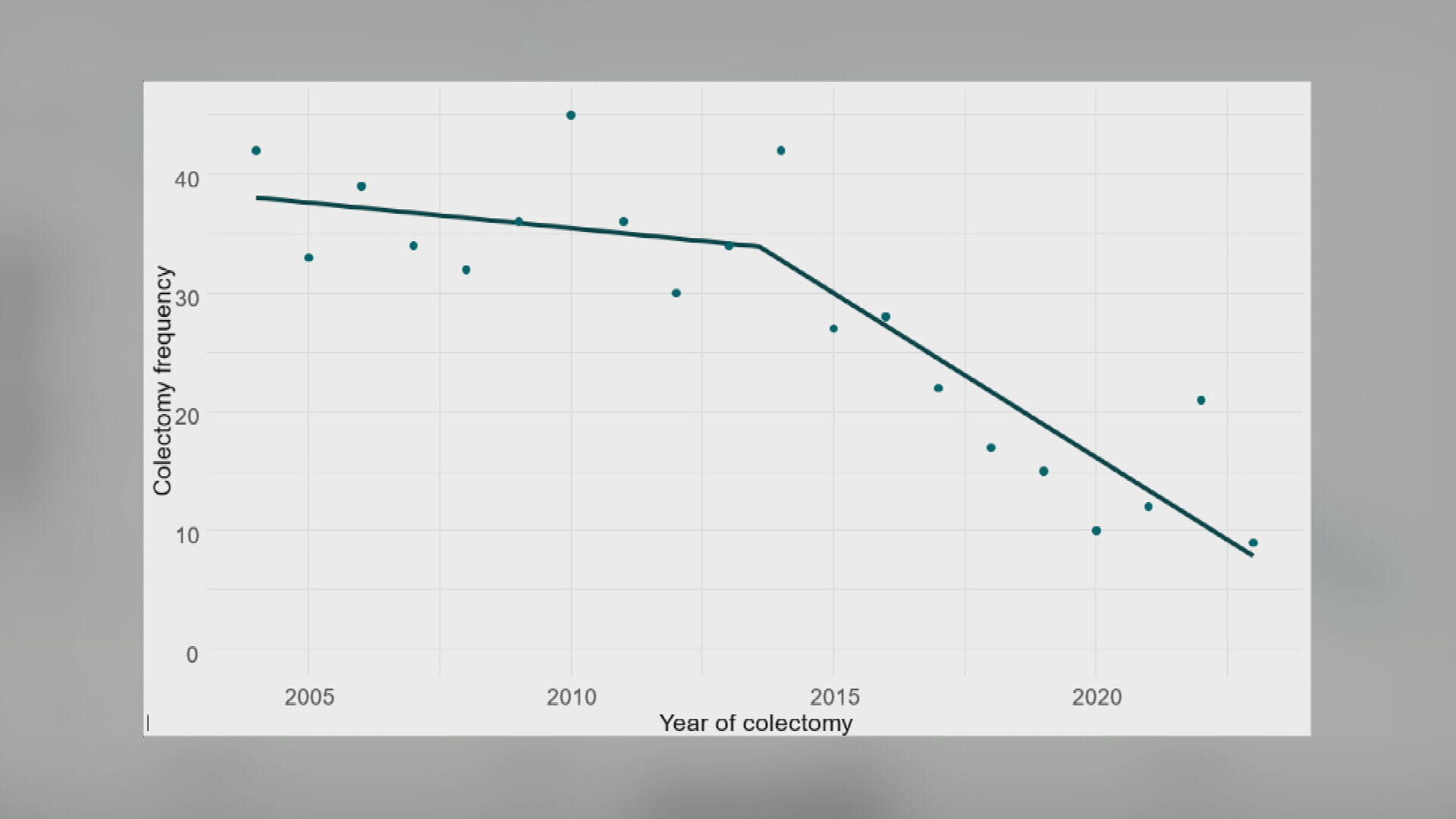
The study collated data over 20 years from people across the Lothian region as and experts say the findings could encourage other health boards to make use of available advanced therapies.
 University of Edinburgh
University of EdinburghOver that time, the number of patients prescribed advanced therapies rose from zero to 115, while colectomy surgeries dropped from 42 in 2004 to just seven last year.
Professor Charlie Lees led the study at the University of Edinburgh’s Institute of Genetics and Cancer.
“This is the first study to document what we’ve been seeing in clinic – that these new treatments are having a big impact on major outcomes,” he said.
He explains that as soon as targeted biologic and small-molecule drugs were being prescribed at scale, the need for colectomy plummeted by more than 80% since 2004.
While surgery remains a necessary option for some patients, Professor Lees said it had been overused in the past due to a lack of alternatives.
“Surgery is a good option for the right patient at the right time, but in the past we went there far too frequently because we hadn’t had other good options.”
Now, with a broader range of highly effective drugs that target different parts of the immune system, doctors can personalise treatment in a way that wasn’t possible a decade ago.
“The UC story over the last ten years has gone from having very few effective drugs, to a situation where we have seven – injectables through the vein, under the skin and new tablet medications.”
He said while there’s no one-size-fits-all solution yet, the results show real progress.
“Patients sequence from one to the other because what we don’t have yet is a crystal ball to find out what drug to give to which patient.
“Sometimes it doesn’t work – try a drug and see how you get on, and move on from there.”
 STV News
STV NewsAmong the new options is filgotinib, an oral medication that has become the most-used first-line therapy since 2021. Unlike some advanced therapies that require infusions or injections, oral drugs offer more convenience at lower costs – an important consideration for NHS services under pressure.
More than 300,000 people in the UK are living with ulcerative colitis. In Lothian, the number of patients doubled over the study period, rising from two in every 1,000 people in 2004 to four in 1,000 by 2023.
Yet, despite this increase, surgical rates have fallen sharply – a trend researchers say began in 2013 when advanced therapy prescribing significantly ramped up.
While there is a clear correlation between the uptake of advanced therapies and decreased colectomy rates over time, the findings cannot prove that the decrease in surgery is caused by access to new treatments, researchers say.
The study also focused on the Lothian region in Scotland, which has ready access to advanced therapies.
Leaders say larger studies are needed to better understand the full picture across areas with fewer resources.
But Professor Lees says the study offers hope for patients diagnosed with bowel conditions that there are options out there.
“UC disrupts people’s lives,” said Professor Lees. “Unpredictable cramp, diarrhoea, going to the toilet eight or more times a day, fatigue – it often leads to psychological problems like anxiety and depression.
“What this enables us to do is say to our patients, we’re doing better with what we have… we can say to other doctors around the country, get on and treat patients with the drugs we have available as they work.
“We can use this information to go to local management systems and regulatory bodies and say it’s really important we have access to therapies that work for our patients.”
Dr Tracey Gillies, medical director of NHS Lothian, welcomed the findings.
“We’re proud of our IBD service and the standards of care it provides,” she said. “Over the years, we’ve invested in staff and made services more accessible, ensuring patients can benefit from advanced therapies and clinical trials.
“Our leading role in academic studies like this helps us to continually evolve and feature in a number of reports as an exemplar.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country