Half of the patients in Scotland affected by a UK-wide E.coli outbreak have been admitted to hospital.
Public Health Scotland said cases are being seen in all age groups but most are among young adults, with 13 cases recorded in Scotland as of June 4.
Half of those recorded cases have required hospital admission, figures showed.
Whole genome sequencing of samples indicates that most of the 113 cases reported across the UK since May 25 “are part of a single outbreak”, the UK Health Security Agency (UKHSA) said.
It said it was working with public health agencies in Scotland, Northern Ireland and Wales, the Food Standards Agency (FSA) and Food Standards Scotland to determine the cause of people’s illness.
All the cases recorded in the outbreak involve Shiga toxin-producing E. coli O145 (Stec), with 81 cases in England, 18 in Wales and one person in Northern Ireland who believes they acquired Stec in England.
The people who have fallen ill range in age from two to 79, with the number of people affected is expected to rise.
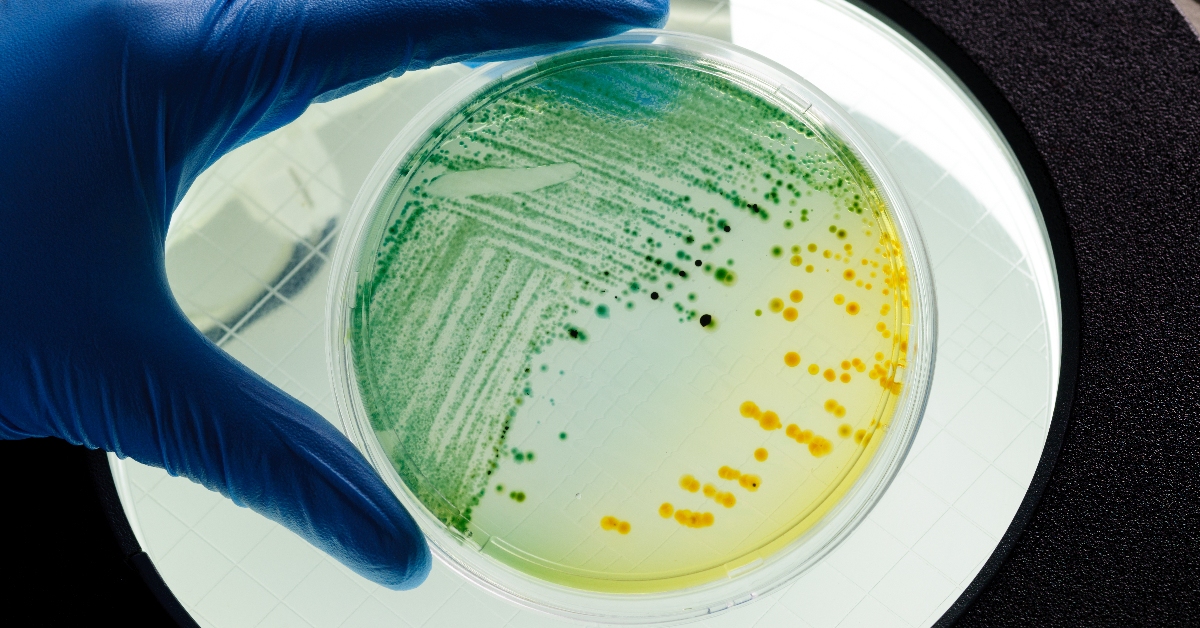
E. coli are a diverse group of bacteria that are normally harmless and live in the intestines of humans and animals.
However, some strains produce toxins that can make people very ill, such as Stec.
People infected with Stec can suffer diarrhoea, and about 50% of cases have bloody diarrhoea.
Other symptoms include stomach cramps and fever.
Symptoms can last up to two weeks in uncomplicated cases.
Jim McMenamin, head of health protection at Public Health Scotland, said: “To help stop infections like E. coli from spreading, we advise regular hand washing using soap and water, particularly after using the toilet and before preparing food.
“People should also use disinfectants to clean surfaces that may be contaminated.
“Anyone experiencing severe and sometimes bloody diarrhoea, stomach cramps, vomiting and fever should call their GP or 111 to seek advice.
“Anyone with diarrhoea or vomiting should avoid attending places such as schools, workplaces or social gatherings until at least 48 hours after their symptoms have ceased.”
Darren Whitby, head of incidents and resilience at the FSA, said it was working to identify the source of the illness “which is likely to be linked to one or more food items”.
Trish Mannes, incident director at UKHSA, said: “If you have diarrhoea and vomiting, you can take steps to avoid passing it on to family and friends.
“NHS.uk has information on what to do if you have symptoms and when to seek medical advice.
“Washing your hands with soap and warm water and using disinfectants to clean surfaces will help stop infections from spreading.
“If you are unwell with diarrhoea and vomiting, you should not prepare food for others while unwell and avoid visiting people in hospitals or care homes to avoid passing on the infection in these settings.
“Do not return to work, school or nursery until 48 hours after your symptoms have stopped.”
People are advised to call NHS 111 or contact their GP surgery if they are worried about a baby under 12 months, a child stops breast or bottle feeding while they are ill, a child under five has signs of dehydration such as fewer wet nappies, and if older children or adults still have signs of dehydration after using oral rehydration sachets.
Help should also be sought if people are being sick and cannot keep fluid down, there is bloody diarrhoea or bleeding from the bottom, diarrhoea lasts more than seven days or vomiting for more than two days, the UKHSA said.
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country


 iStock
iStock

























