A national radiotherapy service described as ‘a total gamechanger’ has treated more young cancer patients in 12 months than was predicted in its first five years.
The molecular radiotherapy suite opened at the Royal Hospital for Children in Glasgow following the multi-million-pound renovation of the Schiehallion unit.
It is one of three centres in the UK delivering specialist treatment and the only one in a dedicated children’s hospital.
Dr Diana McIntosh, consultant paediatric oncologist said: “When I first started seeing children with neuroblastoma 16 years ago, we weren’t able to offer treatment like this.
“There were very few, if any, children who survived. MIBG radiotherapy is a world class treatment that we can offer in Scotland, in addition to all the other therapies, is a complete gamechanger.
“We can only offer this targeted treatment to young people with relapsed neuroblastoma or where the conventional treatments like chemotherapy have not worked but this might potentially change in the future.”

Bashaar Nafiu is the youngest patient so far to be treated in the suite.
The four-year-old travelled with his family from Southampton to Glasgow for two rounds of MIBG therapy.
Taoheed Nafiu, Bashaar’s dad, said: “This is a completely different treatment to the ones he has had in the past.
“Since his diagnosis in February 2021, it has been difficult for my young family, but Bashaar is the one who inspires us. We are just focusing on keeping hope alive and looking at the positives.”
Before his time in the suite, Bashaar had never slept on his own so he had a practice run with a few sleepovers to see how if he would cope.
With Lego, play dough and pirate ships to entertain him, staff say Bashaar “surpassed all expectations” and the radiotherapy was allowed to go ahead.
Behind the reinforced concrete walls and lead doors, the first 48 hours are the most challenging when almost all the young patient’s bodily fluids are radioactive.
After a one-time infusion, which takes about two hours, children must remain in the room for two to five days.
Inside the suite, two specially designed rooms are connected. This means a patient’s parent is able to stay close by and watch from behind protective glass.
While in isolation, they need to take on the bulk of their child’s personal care and they can only spend minimal time together.
It was not only Bashaar, who needed a “practice run” of safety protocols.
His dad, Taoheed had a personal radiation dosimeter to monitor levels and precautions to take to limit his own exposure to the chemicals, targeting his son’s tumour.
Taoheed said: “I realised very quickly normal routines such as bedtime were impossible to maintain in the suite. We were there for five days at a time and I found the toughest part was all the PPE and protective measures you had to follow.
“I’d have just taken it all off and then I’d hear Bashaar say ‘Daddy, I need you’ and I’d have to go and do it all over again.
“When I felt like giving up, I’d look at him and I see him smiling. He never lost his sense of humour and that was really special for me. I thought if he is not giving up then I’m okay.”

When nursing staff need to enter the suite, they work behind a shield.
Senior charge nurse, Emma Sommerville said: “We only come into the room when we really have to and try and to keep as much distance as possible.
“When you are looking after a sick child, your natural instinct is to reach out or give them a cuddle if they are upset but you can move the shield quite close.
“We also try and use some distraction therapies. Our play team is very good. They will have met the child before they come onto the ward to find out their likes and dislikes.
“We have a camera in the room and at the nurse’s station we can keep an eye on them for instance if the parent goes to sleep. We also have an intercom system so we can chat to the patient and the parent if they need a hand.”
The radioactive isotopes used for the treatment are not manufactured in the UK and arrive on site in Glasgow in glass vials inside lead pots packed in dry ice.
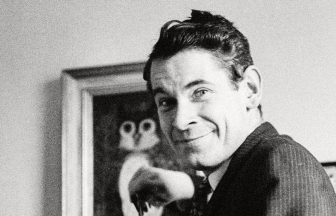
Hugh Wallace, clinical scientist said: “We act as local radiation protection supervisors, and we are here to give advice and assistance to medical staff.
“We must plan our treatments months in advance and need to manage our patient lists very carefully as we have to make sure we have all our orders in for the isotopes weeks ahead of time.
“When a patient is in the suite, what we are looking at it is how quickly the radiation leaves their body.
“This can alter the amount of radiation given in a second treatment to make up the dose to the tumour site. A patient can be in the suite for five days.”
The molecular radiotherapy suite was a new addition to the Schiehallion unit when it reopened last March.
The children’s cancer wards were closed for three years following water bacteria fears.
A multi-million-pound renovation included new filtration and ventilation systems.
With this specialist service, a large multi-disciplinary team is involving in assessing who is suitable. The new suite treated its first child within two months of opening in 2022. Five more quickly followed from across the UK.
Dr Dermott Murphy, consultant paediatric oncologist said: “After years of discussions, it was marvellous to get finally this service off the ground.
“MIBG therapy was originally designed in Glasgow by Tom Weldon so to be able to open this service up for the children of Scotland is a dream come true.
“We had been projecting to Scottish Government we would treat up to five patients in our first five years of delivering molecular radiotherapy. We have already exceeded the number within 12 months.
“It tells us there is a huge untapped level of need and there are children in Scotland who would have waited an inordinate length of time for life saving therapy. ”
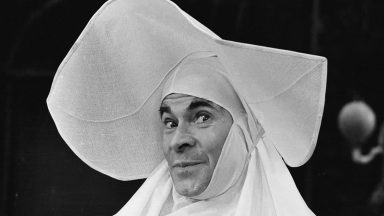
Oliver Duncan, 12, from Inverness was the first to stay in the suite for targeted iodine treatment for thyroid cancer. He says computer games and a prescription of sweets to stimulate his saliva helped while in isolation.
Oliver said: “I thought I was going to turn into the Hulk. All I had to do was take a little tablet that was in a small container, and I was radioactive for two days.
“I could see my mum through the window and talk to her on an intercom, so it wasn’t bad. I just couldn’t touch her.”
Like Bashaar’s dad, Angela was able to stay in a room beside her son during his treatment, where he stayed for two days.
“I was anxious the whole time but I tried not to show Oliver,” she admitted.
“We were like a team. Although I wasn’t in the room with him all the time, it was good that we could be together.
“He was at no point out of my sight so that was a comfort. I felt entirely safe as I had a monitor so I would scan myself every time I went in and out of the room.
“You can get rid for the radiation through sweat, urine, and showering. Oliver did everything by the book and able to speed up the process of getting home to Inverness.
“Oliver’s sister had to move out so we could stay in isolation in our house for a few more days.”
Angela added: “For the immediate future, we have some tests ahead of us. We are hopeful though as they gave Oliver a very high dose of radiation for his age, it was so targeted, it should do the trick. “
Oliver is now looking forward to starting high school after the summer.
Oliver’s consultant, David Colville said: “Up until now we would have to treat paediatric patients within adult services where the facilities were not ideal. Now we have a centralised system that means we can give a high quality of care to our patients in a specialised and children friendly way. “
“The treatments are slightly different. MIBG and the treatment for thyroid cancer both use radio iodine but the way it delivered to the cells is different. Your thyroid gland uses iodine to produce its hormone so by giving radioactivity iodine, it goes to the gland directly.
“With MIBG therapy it targets neuroblastoma by a different process so what we are doing is using tumour biology to target the radiotherapy to the right place.”

Bashaar and his dad did need a second round of MIBG therapy and emerged from extended isolation to be reunited with the rest of the family.
With help from the charity, Calum’s cabin, Bashaar’s mum, and little sister were able to stay in a flat near the hospital for the duration of his treatment.
Taoheed says both he and his son developed a special bond with staff.
“From the nurses to the nuclear medicine staff were always wanting to help. They gave Bashaar more than 100%,” he said. “Bashaar has said it so many times, so they know, we are so grateful.”
Oncologists say MIBG therapy is not only improving outcomes for neuroblastoma patients but also could act a bridge to other treatments.
Dr Diana McIntosh said: “Our aim is that we will see children’s lives prolonged and ultimately cured.
“I hope that MIBG will be more effective than we even think, and we will be able to open it up to offer it to more children not just those who have relapsed or progressed but for the beginning of their treatment as well.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country