Almost 400 children in England have been prescribed weight loss injections on the NHS – the youngest just nine years old, ITV News has found.
Specialist NHS clinics are able to give GLP-1 medications to under-18s if they are living with severe obesity, have serious health complications as a result of their weight, and all other interventions have failed.
“I remember just wishing I looked different – not wanting to go out and not wanting to talk to people,” 15-year-old Lilly told ITV News.
After years of struggling with her weight, despite trying diets and exercise plans, doctors intervened when Lilly’s health became dangerously at risk.
At 13 years old, weighing 20 stone, she was prescribed weight-loss injections. Two years later, she has lost three stone.
“It’s just been completely life-changing,” Lilly said.
“I’ve noticed I can do more exercise and walk further. It’s made me really confident in myself – rather than wishing I was another person.”
Lilly’s mum, Sarah, wants to challenge the stigma associated with childhood obesity.
“This is for children who have fought like hell to change,” she told ITV News. “It’s not for children who stuff their face full of chocolate.”
Previously, she had feared for her daughter’s future.
“I don’t want her to get diabetes or spend the rest of her life struggling to lose weight,” Sarah said.
But since taking the weekly jabs, she has seen her daughter “glowing” with confidence.
“It’s transformational – these medications are so important.”
Childhood obesity is one of the most urgent health issues of our time, with more than one in five children in England living with obesity by the time they leave primary school.
The NHS is now deploying weight loss injections to help tackle the problem.
In England, 36 NHS Trusts run Complications from Excess Weight (CEW) clinics for children living with severe obesity.
Through freedom of information requests, ITV News found that almost half of them, 18 NHS Trusts, have prescribed weight loss injections to children over the last five years.
Our investigation found that a total of 399 children have been given the jabs on the NHS, the youngest aged nine.
Leeds Children’s Hospital runs a specialist clinic for children with severe obesity.
It supports children with weight-related health conditions, such as type 2 diabetes, sleep apnoea and liver disease. Some of the children they treat have a BMI as high as 70.
The majority of their young patients come from deprived areas.

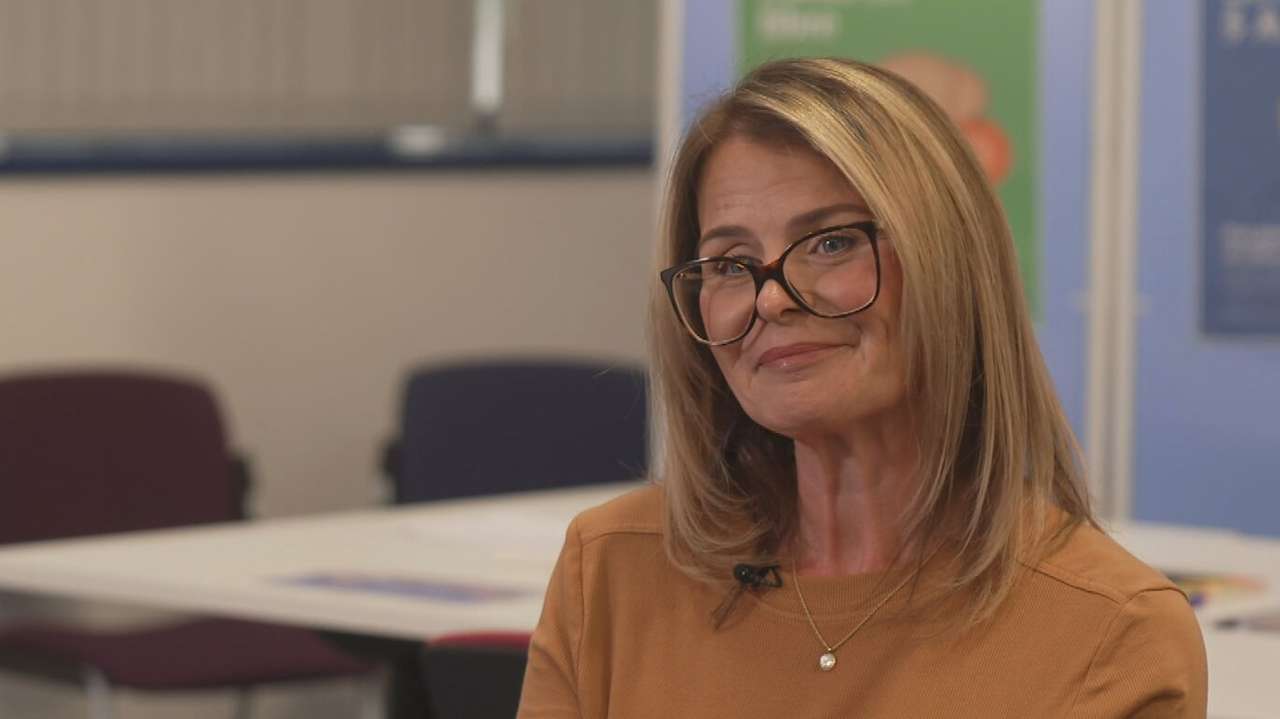
“Poverty plays a massive part – some of our families can’t afford healthier food,” Dr Caroline Steele, a Paediatric Consultant Endocrinologist at Leeds Children’s Hospital, explained.
She told ITV News they take a multidisciplinary approach and weight loss injections, while “important”, are just one part of their “toolkit”.
“Having the support of a social worker and a youth worker and our psychologist, our dietician, our physiotherapist, our nurse as well as medical input is really important,” she said.
Experts say as well as lifestyle and poverty, genetics are also a major factor influencing obesity risk.
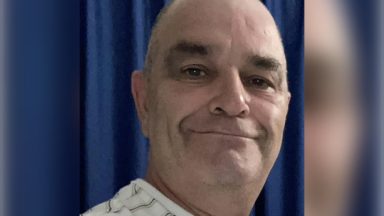
Eddie, 17, has Alström syndrome, a condition which not only causes hearing and vision loss but also weight gain.
Earlier this year, he weighed 19 stone and was at risk of becoming diabetic. With the help of weight loss injections, he’s lost four stone.

“I was trying my best to do sports and eat healthily, but I was barely losing a few grams and then putting them back. It was very, very hard,” Eddie told ITV News.
“It makes me feel way better these days, not being as heavy as before, and I just feel better – they are life-changing,” he said.
But despite the transformative results, some experts are cautious about over-medicalising the next generation.
“For the majority of children, weight loss injections shouldn’t become the go-to,” Bahee Van de Bor, Paediatric Group Chair at the British Dietetic Association, said.
“We really need to think about addressing the root causes,” she added. “What we can offer children in the community and schools to prevent the weight gain in the first place.”

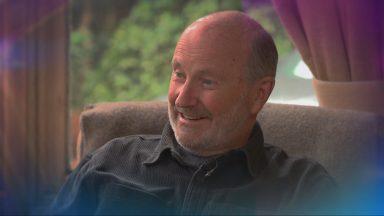
Professor Simon Kenny, National Clinical Director for Children and Young People at NHS England, said: “Obesity can have a devastating impact on children’s health, and it’s fantastic that our specialist NHS clinics have already transformed the lives of thousands of young people through a holistic approach – supporting them to lose weight, live healthier lives and improve their mental health.
“Alongside personalised support to achieve healthy lifestyle changes, weight loss drugs are playing an important role for some children, and these are only prescribed following careful assessment by paediatric specialists.
“Interventions such as behavioural coaching, specialist dietary advice and mental health support remain the cornerstone of care for children, but weight loss treatments can also help to prevent or reverse serious conditions such as type 2 diabetes and obstructive sleep apnoea, where lifestyle interventions alone have not been sufficient.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country